Nuestros estudiantes dicen sobre nosotros
WELCOME
-
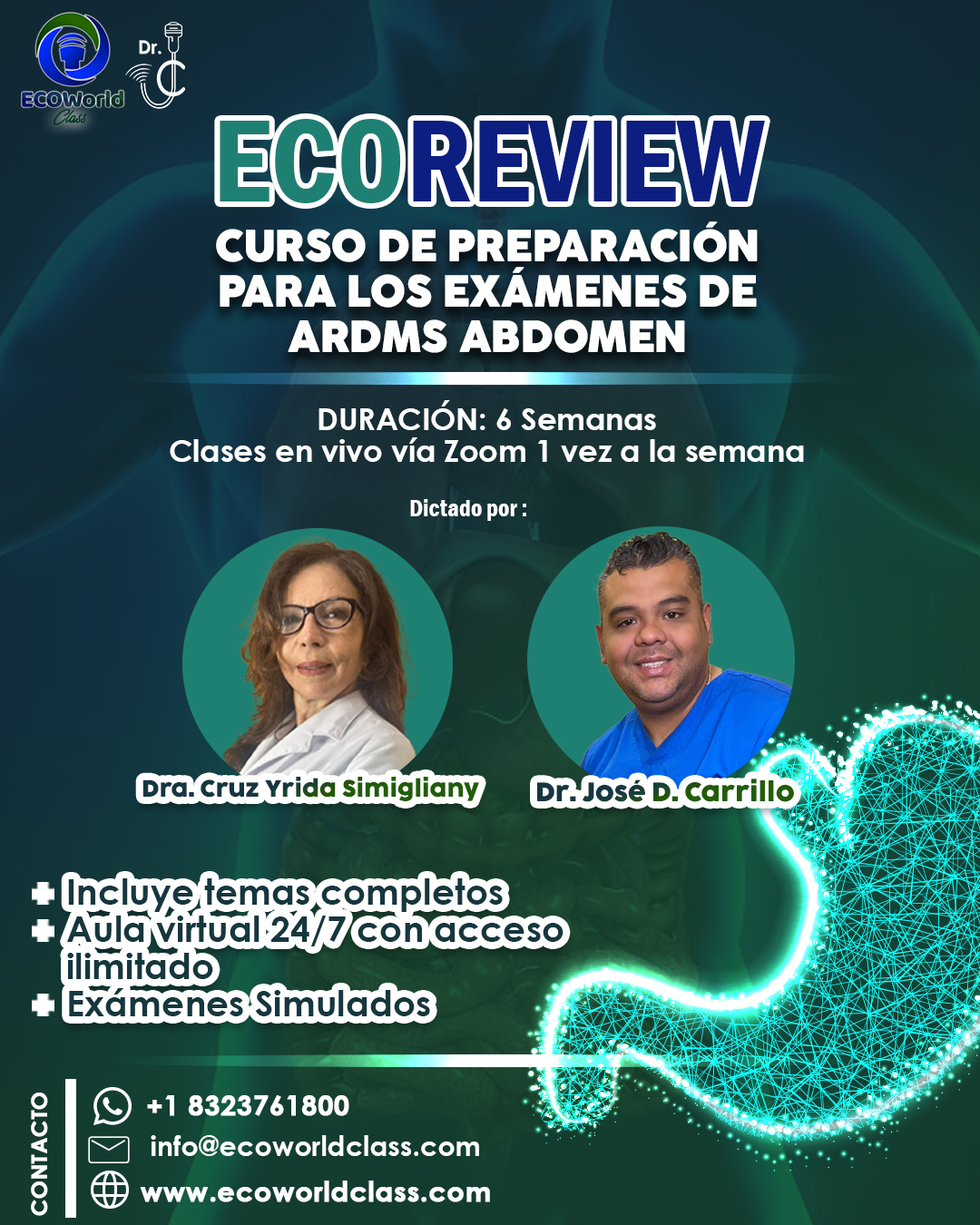
Bienvenidos al Curso de Ultrasonido Ecoreview Abdomen
01:21 -
EXPLICACION DE COMO MANEJAR EL AULA VIRTUAL
08:14
WEEK 1
-
ABDOMEN ULTRASOUND PHYSICS
01:49:48 -
CHAPTER I
-
LIVER
01:53:07 -
LIVER CAPITULO II
01:14:06 -
CHAPTER II LIVER
-
practica evaluacion del lobe left hepatic
04:28 -
Practica Liver complete
05:21 -
Liveclass week I
02:28:44
WEEK 2
🟢 CHAPTER 3: NORMAL AND PATHOLOGICAL GALLBLADDER
🔬 Normal Anatomy
The gallbladder is a pear-shaped or saccular organ located in the gallbladder fossa, situated between the right hepatic lobe and the quadrate lobe of the liver. It consists of three parts: the fundus, body, and neck. Its main function is to store and concentrate bile, releasing it after meals to aid in digestion. In fasting patients, the gallbladder is typically distended and easier to evaluate.
Its normal length ranges from 7 to 10 cm, and the wall should measure ≤ 3 mm. An anechoic lumen without internal echoes is considered normal. The gallbladder receives blood supply from the cystic artery, which branches off the right hepatic artery. Normally, the cystic duct is not visualized unless dilated.
📏 Key Measurements
A wall thickness greater than 3 mm raises suspicion for inflammation. A gallbladder with no internal content and thin walls is considered normal. Any visible cystic duct dilation should be evaluated further, as it is not usually seen unless abnormal.
🟡 Cholelithiasis (Gallstones)
Gallstones appear as echogenic foci with posterior acoustic shadowing. They usually move when the patient is repositioned. Gallstones are the most common cause of gallbladder disease and may lead to obstruction and cholecystitis.
🟤 Biliary Sludge
Biliary sludge consists of low-level echoes that do not produce shadowing. It tends to layer dependently and shifts slowly with patient movement. Sludge is associated with bile stasis and may precede gallstone formation.
🌱 Gallbladder Polyps
Polyps are non-shadowing, non-mobile echogenic masses attached to the wall. They are usually benign, especially if smaller than 10 mm. If larger or rapidly growing, further evaluation is required due to the risk of malignancy.
🌀 Adenomyomatosis
Adenomyomatosis is a benign condition involving focal or diffuse wall thickening and intramural diverticula known as Rokitansky-Aschoff sinuses. It produces characteristic comet tail artifacts or ring-down artifacts, often in the gallbladder body.
🔥 Acute Cholecystitis
This condition is most often caused by cystic duct obstruction due to a gallstone. Sonographic findings include gallbladder wall thickening (>3 mm), positive sonographic Murphy's sign, pericholecystic fluid, and gallbladder distention. Shadowing gallstones and sludge are often present.
⚠️ Acalculous Cholecystitis
This is an inflammation of the gallbladder without gallstones, typically seen in critically ill or hospitalized patients. Diagnosis can be challenging, but ultrasound may show wall thickening, distention, and fluid, even in the absence of calculi.
💨 Emphysematous Cholecystitis
This life-threatening form of cholecystitis is caused by gas-producing bacteria. It presents with echogenic foci in the wall or lumen with dirty shadowing and reverberation artifacts due to gas. It carries a high risk of perforation and requires urgent intervention.
🧟 Gangrenous Cholecystitis
A complication of acute cholecystitis, gangrenous cholecystitis involves necrosis of the gallbladder wall. Findings include irregular wall thickening, sloughed membranes, intraluminal debris, and absence of Murphy's sign. It is associated with a higher risk of perforation.
🎗️ Gallbladder Carcinoma
Gallbladder cancer is rare but highly aggressive. Sonographic signs include a mass replacing the gallbladder, focal wall thickening, or a large non-mobile polypoid lesion. It is often associated with porcelain gallbladder and gallstones.
🔵 CHAPTER 4: BILIARY TREE (CBD and Intrahepatic Ducts)
🧠 Anatomy and Physiology
The common bile duct (CBD) is formed by the junction of the cystic duct and the common hepatic duct. It courses posterior to the pancreatic head and drains into the duodenum at the ampulla of Vater. On ultrasound, the CBD is typically visualized anterior to the portal vein in the portal triad.
The normal diameter of the CBD is up to 6 mm in adults under 60 years. One may add 1 mm per decade of life after age 60. In post-cholecystectomy patients, a CBD measuring up to 10 mm may still be considered normal.
🪨 Choledocholithiasis
Stones within the bile duct appear as echogenic foci that may or may not cast shadowing. They are usually associated with dilated intra- and extrahepatic ducts. Symptoms include jaundice, pain, and fever (Charcot’s triad in cholangitis).
🧬 Cholangitis
Cholangitis is an infection of the bile ducts, often caused by obstruction (e.g., from a stone or tumor). Ultrasound may show dilated ducts, thickened duct walls, and biliary debris. Clinical signs include fever, jaundice, and RUQ pain.
🎗️ Cholangiocarcinoma
This is a malignant tumor of the bile ducts, commonly at the hepatic duct bifurcation (Klatskin tumor). Sonographically, it appears as a mass at the hilum with proximal ductal dilation and no visible distal obstruction.
🛠️ Iatrogenic Injury / Strictures
Following surgery (e.g., cholecystectomy), the bile ducts may develop strictures or leaks. Ultrasound can reveal focal ductal dilation or fluid collections, and further imaging (e.g., MRCP or HIDA scan) is often required.
🪱 Biliary Parasites (Ascaris)
Parasitic infections such as Ascaris lumbricoides may appear as mobile tubular structures within the ducts. They are hypoechoic with echogenic borders and may move on real-time imaging.
🧪 Important Signs and Artifacts
Double Barrel Sign: The CBD and portal vein appear as two parallel anechoic tubes in the portal triad.
Shotgun Sign: Refers to dilated intrahepatic ducts running parallel to portal veins.
WES Sign (Wall-Echo-Shadow): Classic appearance of a stone-filled gallbladder; gallbladder wall, echogenic line from stones, and posterior shadowing — no visible lumen.
✅ Key RDMS Exam Takeaways
A CBD measuring >6 mm is considered abnormal, unless the patient is elderly or has had a cholecystectomy. Use color Doppler to differentiate ducts from vessels. A positive Murphy's sign with wall thickening is highly suggestive of acute cholecystitis. A non-shadowing, non-mobile lesion should raise concern for a polyp or malignancy. If the bile ducts are dilated without a visible cause, further imaging such as CT, MRCP, or ERCP is recommended.
-
Chapter 3
02:16:57 -
Chapter 4
01:14:47 -
PRACTICA LIVER COMPLETE + GALLBLADDER
06:58 -
LIVE CLASS 06/18/2025
01:57:46 -
QUIZ GALLBLADDER
-
QUIZ THE BILE DUCTS
-
PRACTICA OPTIMIZAR UNA IMAGEN
16:09 -
GALLBLADDER PROTOCOL
11:40
WEEK 3
🎓 Hello colleagues, welcome to a new study week in the ECOREVIEW RDMS-Abdomen course.
🗓️ This week we will be covering three key topics for the certification exam:
⸻
🔷 1. Pancreas
The pancreas is a retroperitoneal organ with both endocrine (insulin, glucagon) and exocrine (digestive enzymes) functions.
🧠 Essential exam points:
Echogenicity: Typically hypoechoic or isoechoic compared to the liver.
Common pathologies:
Acute pancreatitis: Enlarged, hypoechoic pancreas with possible fluid collections.
Chronic pancreatitis: Small, echogenic pancreas with calcifications.
Neoplasms: Adenocarcinoma (commonly in the head), associated with dilated pancreatic duct (Wirsung).
Pancreatic duct (Wirsung): Normally 13 mm
Reversed (hepatofugal) portal flow
Collateral circulation: Dilated gastric, splenic, or paraumbilical veins.
Splenomegaly: An indirect sign.
Ascites may also be present.
⸻
📌 Remember: These entities are highly tested in the RDMS-Abdomen exam. Be prepared to identify their ultrasound characteristics, correlate them with clinical findings, and apply diagnostic criteria.
See you in class to review images, exam-style questions, and clinical correlations. Let’s give it our all this week! 💪📚
-
PANCREAS
01:10:29 -
SPLEEN
51:36 -
SPLEEN (copy)
51:36 -
AORTA ABDOMINAL
-
VIDEO PRACTICO I
12:39 -
live class 06/25/2025
01:43:34 -
PANCREAS
-
SPLEEN
WEEK 4
📋 Ultrasound Overview: Abdominal Aorta, Kidneys, and Adrenal Glands (with Emojis)
1. Abdominal Aorta 🏥
📐 Anatomy & Segments: Infradiaphragmatic portion from diaphragm to iliac bifurcation.
📏 Normal Diameter: 3 cm dilation)
Dissection (echogenic intimal flap)
Mural thrombus (echogenic wall adherent clot)
2. Kidneys 🩺
📏 Normal Measurements:
Length 9–12 cm; cortical thickness > 1 cm
Cortex is more echogenic than medulla
🔍 Technique:
Patient in lateral decubitus
3–5 MHz convex probe in coronal & transverse planes
💧 Common Findings:
Hydronephrosis: dilated pelvicalyceal system
Nephrolithiasis: echogenic stones with shadowing
Simple cysts: anechoic, thin walls, posterior enhancement
Solid masses: heterogeneous echoes, abnormal Doppler flow
📈 Doppler Parameters:
Interlobar artery PSV 0.7 suggests stenosis)
3. Adrenal Glands 🌟
📍 Location & Shape: Superior–medial to renal poles; triangular on right, semilunar on left.
🔍 Technique:
5 MHz convex probe
Oblique coronal plane over kidney
Contralateral lateral decubitus
🎨 Normal Appearance:
Length 2–4 cm; thickness < 1 cm
Hypoechoic cortex with echogenic medulla
⚠️ Pathologies to Recognize:
Adenoma: small, homogenous, stable nodule
Pheochromocytoma/Carcinoma: heterogeneous, hypervascular mass
Metastases: multiple lesions, rapid growth
Hyperplasia: diffuse bilateral enlargement
🔑 ARDMS/RVT Exam Tips:
Memorize normal size ranges and probe settings.
Use Doppler to assess renal artery velocities and resistive indices.
Identify and differentiate cystic vs. solid lesions and recognize vascular patterns.
Good luck on your exam! 🚀
-
ABDOMINAL VASCULATURE
01:17:34 -
ABDOMINAL VASCULATURE
-
THE URINARY TRACT
01:47:44 -
THE URINARY PART II
01:21:53 -
THE URINARY TRACT
-
ANDRENAL GLANDS
46:42 -
ADRENAL GLANDS
-
CLASS IN LIVE
02:33:42
EXAMEN REPORT
Hello, dear students! 🌟 Welcome to this module, thoughtfully designed to help you master the art of writing clear, concise, and professional ultrasound reports before sending them on to the radiologist. 📋✨ Here, you’ll learn how to highlight the most important findings, record accurate measurements, and draw appropriate conclusions—all in a way that showcases your technical expertise.
Throughout this module, you’ll practice:
• Describing organ size and echotexture with precision 🔍
• Noting the presence or absence of masses, cysts, stones, or sludge 🏥
• Measuring structures like the gallbladder wall and common bile duct, and interpreting those values 📏
• Reporting on vascular flow patterns, such as hepatopetal portal vein flow 🌊
By the end of this exercise, you’ll be able to confidently compose a complete, well-structured report that reads smoothly and provides the radiologist with all the data they need. Let’s get started—your future self (and your patients!) will thank you. 🙌🏼😁
Example : The liver measures 13.2 cm and demonstrates a homogeneous echotexture without evidence of intrahepatic masses or cysts; increased echogenicity from fatty infiltration consistent with Grade I steatosis may be present. The gallbladder wall is thin at 0.30 cm, the lumen is anechoic, and no gallstones or sludge are identified. The common bile duct measures 0.78 cm in diameter, within normal limits, and shows no dilatation. The portal vein exhibits hepatopetal flow with a diameter of 0.93 cm, also within expected parameters. All findings are consistent with a normal ultrasound examination of the liver, gallbladder, and biliary tree.
-
1 REPORT
-
REPORT II
-
REPORT III
EVALUATION NUMBER 1
Estimados estudiantes, atención:
– La Evaluación Nº 1 constará de 70 preguntas de estilo RDMS.
– Dispondrán de 1 minuto para responder cada pregunta.
– No habrá reintentos: una vez enviado el examen, no podrán repetir ninguna pregunta.
Les recomiendo gestionar bien su tiempo: si una pregunta les lleva más de un minuto, continúen avanzando y regresen a ella —en la medida de lo posible— dentro del tiempo asignado. ¡Éxito en su preparación!
-
QUESTION TYPE RDMS